General Concept
Our lab focuses on the development of new therapy concepts for solid tumors with only poor treatment options to date. The translational research concept requires close cooperation with clinical partners as well as various other academic disciplines like synthetic and analytic chemistry. The investigated therapy-resistant tumor types include primary brain tumors, melanoma, bladder cancer, and malignant lung diseases.
Development of New, Innovative Tumor Therapies with Reduced Side Effects
The project performed in frame of an inter-university research cluster for translational cancer therapy development supported by the Medical University of Vienna and the University of Vienna, aims at the development of new, well-tolerated cancer therapeutics.
In close collaboration with the Institute of Inorganic Chemistry (Head: Prof. Bernhard Keppler) completely new anticancer drugs are designed as well as classical chemotherapeutics and tyrosine kinase inhibitors get optimized – based on prodrug strategies for tumor-specific activation – with regard to drug efficacy and reduction of adverse effects.
Within this context we also develop therapeutics that, upon activation within the tumor tissue, release besides the active anticancer substance additional ligands like resistance modulators (e.g. a glutathione synthase inhibitor) or immune activators (e.g. a STING agonist).
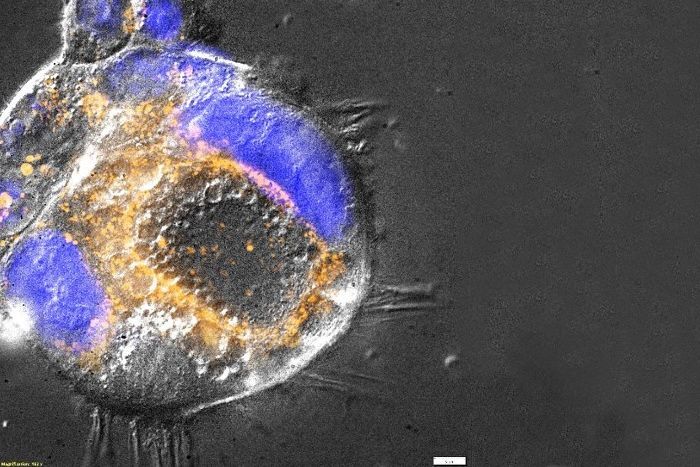
For one of our newly designed therapeutics, following patent registration, already a spin-off company has been founded. A further substance (BOLD-100) is currently tested in clinical phase I/II trials in the US and Canada. For this first-in-men drug we could identify deregulation of the cellular sugar and lipid metabolism followed by epigenetic reprogramming as the main mode-of-action (Baier et al. Pharmaceutics, 2022). Accordingly, Figure 1 shows accumulation of lipid droplets in a colon cancer cell with acquired BOLD-100 resistance
Molecular and Pharmacological Factors of Therapy Resistance
Both intrinsic and acquired therapy resistance unfortunately represent major obstacles for any form of systemic cancer therapy. Thus, besides the development of new drugs, our lab focuses on the detailed identification and elucidation of resistance phenomena and on strategies to overcome therapy failure. Even modern targeted therapeutics, after an initial success phase, often rapidly loose efficacy.
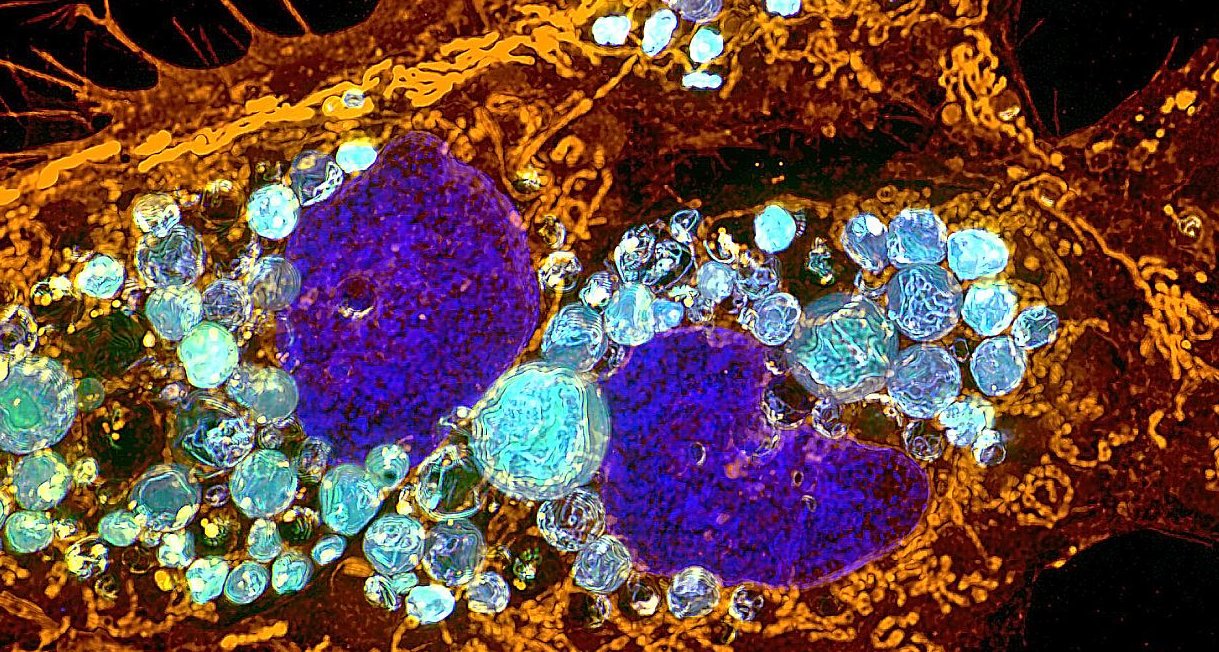
Apart from efflux pumps and classical detoxification mechanisms, therapy failure can be caused e.g. by altered intracellular drug distribution. Recently, we discovered that Nintedanib, a substance used for the treatment of lung cancer, can be trapped in lysosomes by protonation occurring in the acidic pH milieu of these organelles (Englinger et al. J. Exp. Clin. Cancer Res. 2017). Such, the drug cannot reach the cancer-driving receptor tyrosine kinases located at the cell membrane and remains ineffective. The high Nintedanib concentrations in lysosomes even result in formation of green fluorescent crystalline structures (Figure 2). As a strategy to overcome this type of resistance we currently explore combination strategies with drugs that shortly can increase the lysosomal pH-value
Identification of New Therapy Targets – Focus on FGFR Molecules
In cooperation with several clinical partners we work on the evaluation of new cellular targets that might improve therapy options for patients with difficult-to-treat or rare tumor types. Central target molecules represent her the receptors of fibroblast growth factors (FGFR1-4), which in many cases drive malignant transformation and progression.
Within a cooperation with the Department of Neurosurgery, AKH Vienna, we could recently show that FGFR4 acts as a major tumor driver in a subgroup of glioblastoma cases and might serve as a promising therapeutic target.
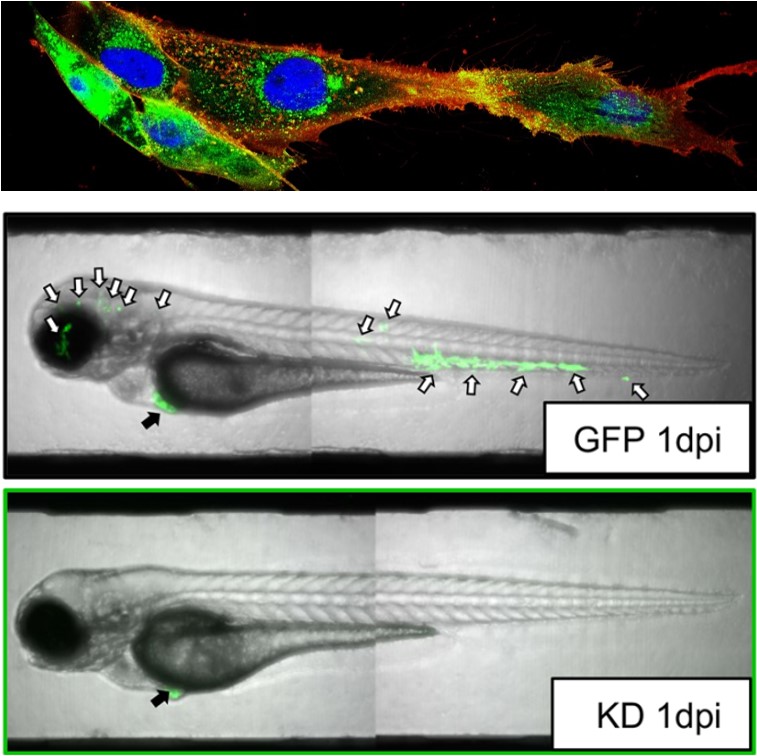
Figure 3 shows localization of FGFR4 in a glioblastoma cell model established from patient surgical material and the massive impact of an FGFR4 blockade on cancer cell invasiveness e.g. in the zebrafish model (cooperation with the CCRI, Vienna) (Gabler et al. Acta Neuropath. Comm. 2022).
In close collaboration with the Department of Pediatrics and Adolescent Medicine, AKH Vienna, we were able to prove successfully the efficacy of comparable new treatment approaches in a few children with pediatric brain tumors like e.g. ependymoma (Lötsch et al. Acta Neuropath. 2021).