Food and Hepatocarcinogenesis
In Austria and other industrialized countries, the prevalence of overweight, type II diabetes and/or the metabolic syndrome are steadily increasing. These dietary diseases are important risk factors for the development of hepatocellular carcinoma. The aim of our research is the identification of dietary factors that are causally involved in hepatocarcinogenesis. Currently we are investigating the role of fatty acids, enhanced blood levels of insulin and of chemical compounds contaminating the food chain.
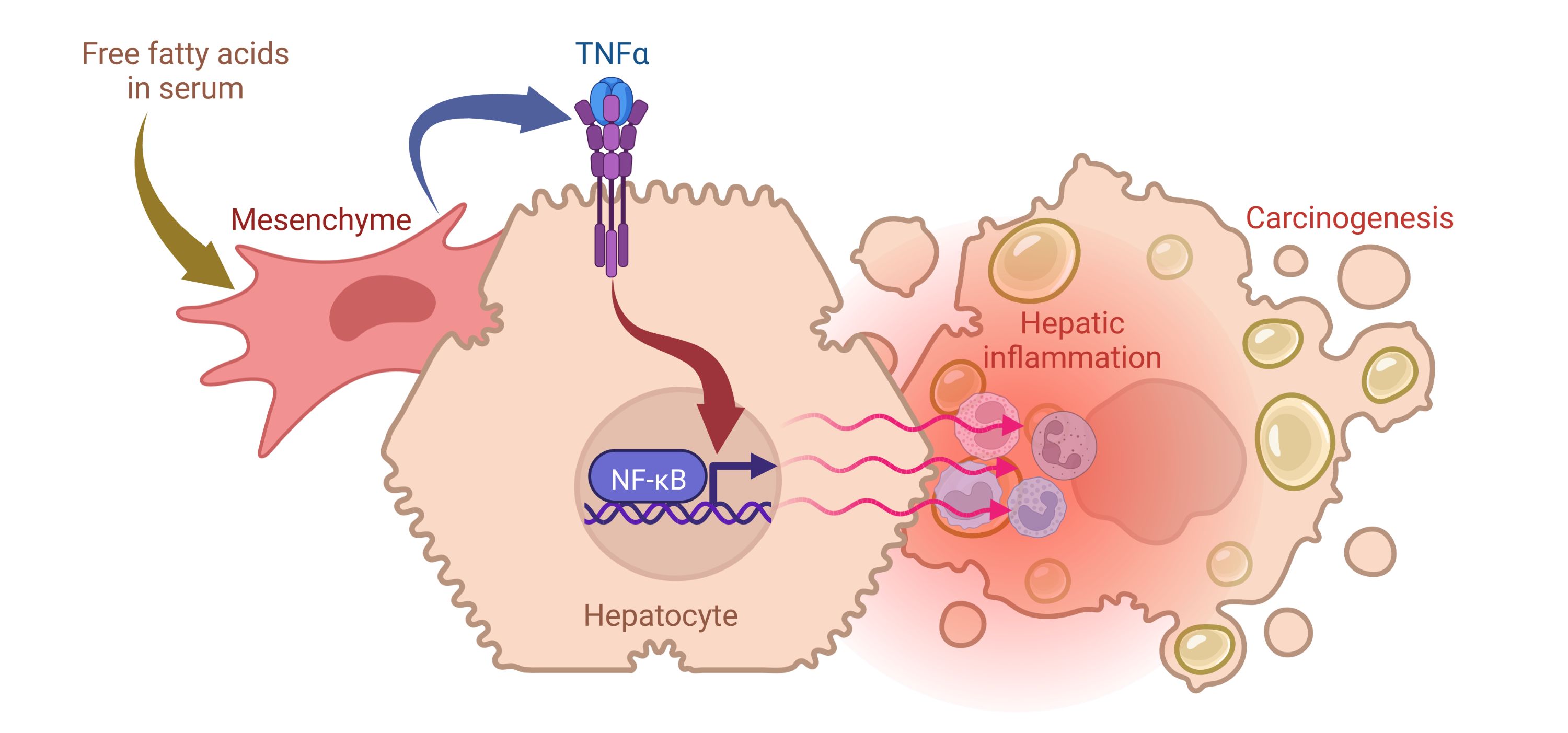
Fatty acids and hepatic inflammation
Hepatocellular carcinoma almost always develops in a chronically inflamed liver. A persistent hepatic inflammation causes enhanced cell turnover. As a result, deregulated production and aberrant signaling of growth factors, such as fibroblast growth factors (FGFs), may lead to altered cell growth, differentiation, and apoptosis. The result may be formation and selection of premalignant hepatocytes, which increasingly lose normal growth control and may give rise to cancer.
Different factors may cause chronic hepatic inflammation, such ethanol abuse or chronic viral infections. Furthermore, excessive food consumption is frequently associated with enhanced lipid storage in the liver (hepatic steatosis) and the risk for the development of hepatitis (non-alcoholic steatohepatitis, NASH). The mechanisms underlying the progression of a fatty liver to NASH are not completely known.
We are currently investigating whether increased serum levels of free fatty acids, as occurring frequently in obesity or in patients suffering from diabetes type-2/metabolic syndrome, may trigger the outbreak of hepatic inflammation. We found that free fatty acids stimulate mesenchymal liver cells to release pro-inflammatory tumor necrosis factor α (TNFα), which activates the NFkB. This signal cascades triggers the development of hepatic inflammation and interferes with pro-apoptotic signal transduction pathways. As a consequence, enhanced survival of premalignant hepatocytes supports indirectly growth of preneoplasia and enhances the probability for development of hepatocellular carcinoma.
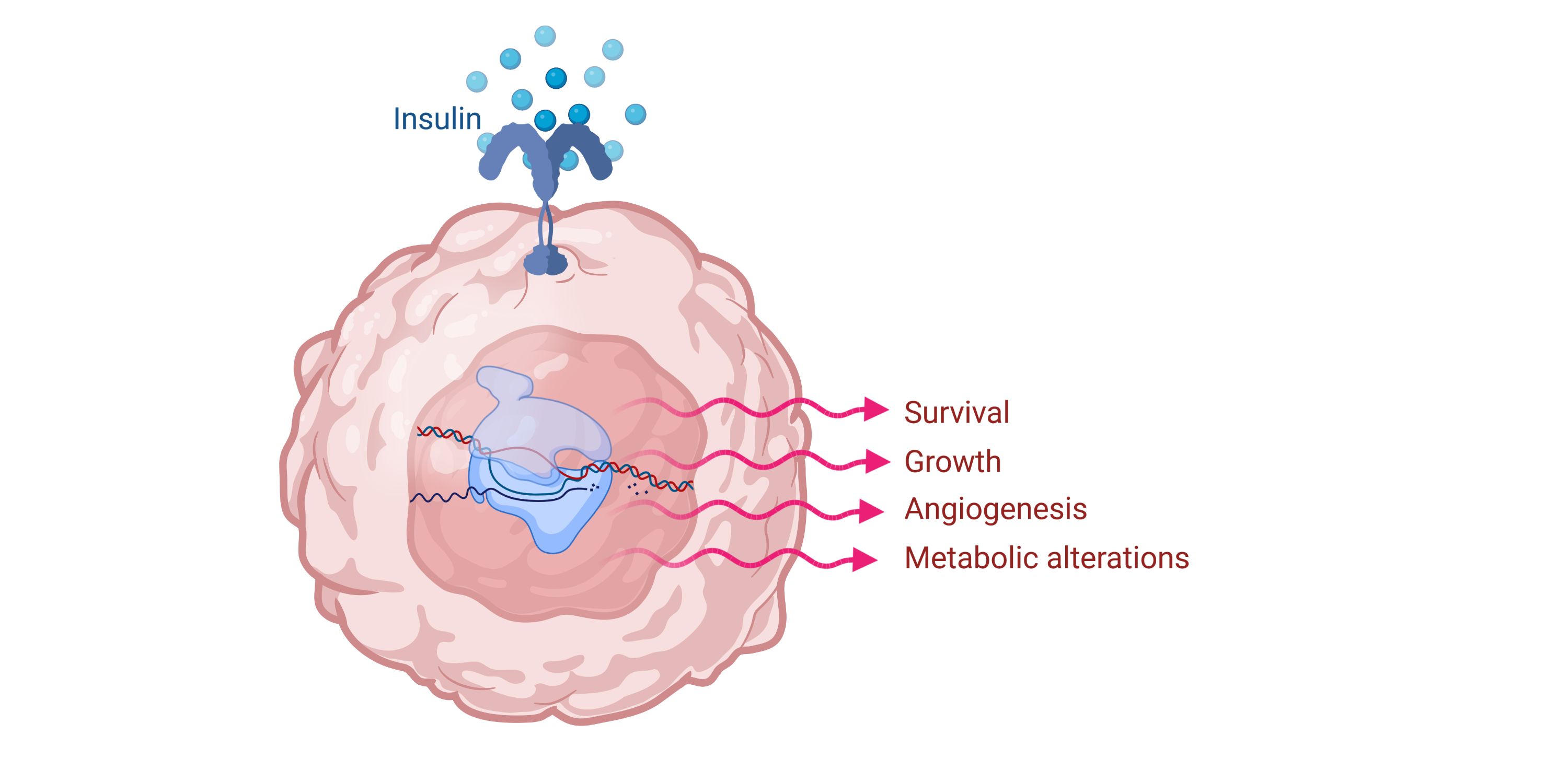
Insulin and hepatocarcinogenesis
Patients with hyperinsulinemia and/or diabetes type-2 are at an increased risk to develop hepatocellular carcinoma. In a current project we are investigating whether insulin is causally involved in hepatocarcinogenesis.
Several insulin-regulated genes, involved in the carbohydrate- or lipid metabolism, showed overexpression in liver tumor prestages. Insulin treatment led to enhanced colony formation, cell migration of liver cancer cells and stimulated neoangiogenesis. The results indicate that insulin might contribute to hepatocarcinogenesis due to effects on metabolic gene expression and the development of a malignant phenotype.
Carcinogenic activity of chemical compounds in the liver
Chemical compounds are the dominant cause of human cancer. The focus of our research is to elucidate how cancer is induced by chemical compounds in food, such as contaminants in the food chain. We characterize the hepatocarcinogenic activity of such compounds on cultured liver cells, the intact organ, and liver cancer prestages at the cellular and molecular level. These experimental data - together with literature data on exposure analyses and dose-response analyses – are a valuable contribution for (i) the assessment of the risk to develop hepatocellular carcinoma in case of exposure and (ii) for the development of cancer-preventive measures.